Pain
‘Does it hurt?’ ‘How long until the pain goes away?’
Those are common questions that I often hear, and that I had myself. I can say that results have not met expectations… in a good way. Right out of surgery you would think it would hurt like hell. You would think the pain would be constant. It really didn’t. I was sore, very sore, but not really in pain, per se. Of course there were some really good pain meds being pumped into me via the IV, so I’m sure that had something to do with it.
It did hurt when I would try to sit up, or twist my upper body. Getting in and out of bed was a chore, and in the first few days I really needed help doing it. This was tough for me. I’m someone who always prided them self on being independent. I’m a big boy, I could get up and go to the bathroom on my own, right? Well, no, I couldn’t. I needed help. At first from nurses, two in ICU, one in the regular room, but later as I improved Missy was able to help me alone. Then, once back in bed I wouldn’t be up high enough so two nurses would have to ‘adjust’ me. One on each side, they’d grab the sides of a pad that I was laying on, 1… 2… 3… *heave!*, and that would work. My bed could be adjusted up now and I could go back to sleep.
It hurt when I coughed, which I was warned about from everyone, but not as bad as I had been warned. A local charity gave me a heart pillow that would become my ‘security pillow’ for the foreseeable future. Coughing is a big deal. You hold this tightly to your chest when you cough, it helps manage the immediate pain somewhat, and you’re encouraged to cough often to clear your lungs of stuff so you don’t get pneumonia. Breathing clearly is one of everybody’s foremost concerns in your recovery for this reason.
What does hurt, and what no one had really warned me about, is sneezing. One person did warn me, after I mentioned it to them, to “let it fly” and not hold it in, and now I know why. When you hold it in it creates a great pressure and strain on your lungs and chest, and they don’t need that right now.
By the time I came home, there was virtually no pain at all, except for coughing and sneezing. The soreness lasts quite awhile, and you move slowly everywhere and for everything. Two days after I got home I unloaded the dishwasher, and that single effort wiped me out and left me in some pain and soreness, so I took a nap.
As I sit here writing this almost three weeks later my chest is still sore, but much of that is the skin around the incision tightening as it heals, which it is doing quickly. Last couple days I have had a few instances where it felt like my heart ‘jumped’, and would sometimes cause a reflex in my arm and/or leg. This is new. Some internet research indicated that it might be AFib (Atrial Fibrillation), which is fairly common after heart by-pass surgery. I am on meds to prevent blood clots, and AFib usually goes away fairly quickly in this case. I have a doctor appointment with my surgeon for a check-up later today and will ask about it.
The two very small incisions in my left leg have been fine. The long incision on my inner left arm has been the most problematic. It’s appeared more inflamed, but my cardiologist said it was fine. It gets sore as well, partially for the same stretching reasons, but also partly because it keeps rubbing against things, primarily my stubbly chest and stomach hair as it grows back in.
Both my chest and arm incisions are hypersensitive, though. I do not enjoy not wearing a shirt, but have had to go shirtless a lot here at home because a shirt brushing up against an incision is quite irritating, and if it goes on for too long they do begin to hurt.
Pain Medications
Prior to surgery I was given some kind of medication to take on a daily basis that I call “mini nitroglycerine”. If I remember correctly this was to expand my arteries, or something like that. It gave me severe headaches, which I had been warned was a possibility, so I stopped taking it after about 3 days.
I do not remember what pain med they gave me through the IV after surgery. I was taking Oxycodone and Tylenol in pill form after surgery. The Oxycodone was interesting. I had some strange dreams on that stuff. One while in the hospital had me dreaming of scrolling Facebook on my phone, and I somehow knew my hand was up near my face actually making scrolling motions. I told myself to stop doing that, but I kept doing it. I would have thought nothing of it, but Missy told me about it the next morning, and confirmed that not only did she see my hand making the scrolling motion, but my legs were moving, too, kind of like how a dog runs in its sleep.
The second day after I got home I started getting sick. Discharge instructions said to call the nurse’s station if any issues so I did. They said call my family doctor, so I did. They said call my surgeon’s office, so I did. They initially didn’t want to deal with it, but when I explained more she went and consulted with my surgeon and he said to discontinue my two anti-biotics and the Oxycodone, as either were known to potentially cause this. I did so, and I stopped getting sick. Before we ended the call, though, I was instructed that any other questions should go to my family doctor. 😐 Thanks.

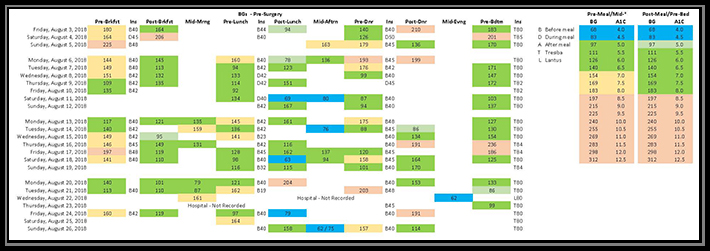 My endocrinologist today said that I have provided too much information. It’s overwhelming and hard to narrow anything down, but that’s jumping ahead a bit.
My endocrinologist today said that I have provided too much information. It’s overwhelming and hard to narrow anything down, but that’s jumping ahead a bit.